Get in touch
-
Additional Tax Relief available for “R&D Intensive” SMEs
Consulting
News Article
Find out more about the enhanced tax relief that R&D-intensive, loss-making SMEs will receive under the new merged R&D tax relief scheme introduced by the Government on April 1st 2024. Read on...
12 April 2024

-

Advancements in Additive Manufacturing for Aerospace Components
Innovation & New Technology
Consulting
News Article
14 March 2024
With every material breakthrough, every design innovation, and every step towards more sustainable manufacturing practices, Additive Manufacturing reaffirms its role as a cornerstone of aerospace engineering and manufacturing.

-

Finance Act 2024 - Impact of new R&D tax legislation
Consulting
News Article
29 February 2024
The biggest shake-up to the R&D tax scheme since its inception is now consecrated in law. The rules governing the single RDEC scheme and the R&D Intensive SME scheme are now set in legislation. Although the new schemes do result in some minor simplifications, these rules also bring about complexities that we advise companies to seek immediate professional advice on. Read on...

-

Capital RDAs or Capital Allowances? A Guide to Maximising the Allowances on Offer
Consulting
News Article
19 February 2024
Following recent changes both to the R&D tax relief scheme and to Capital Allowances, many companies are confused about which pot to claim from, in order to maximise the tax breaks they can take advantage of. Our Guide to Maximising the Allowances on Offer is worth a read if you undertake R&D

-

SOLIDWORKS Generates Positive Reaction at MoltexFLEX
Solutions
Case Study
16 February 2024
MoltexFLEX, has been diligently crafting the 'Flex Reactor', a graphite moderative marvel poised for mass deployment and ready to disrupt fossil fuel dominance. We visited the team to find out how SOLIDWORKS has helped them develop their game changing green technology...

-

March Year End: Fail to Prepare, Prepare to Fail
Consulting
News Article
18 January 2024
Read our guide for a reminder to secure your claims before the deadline and also to find out more about how to prepare for the upcoming changes in R&D tax incentives.

-

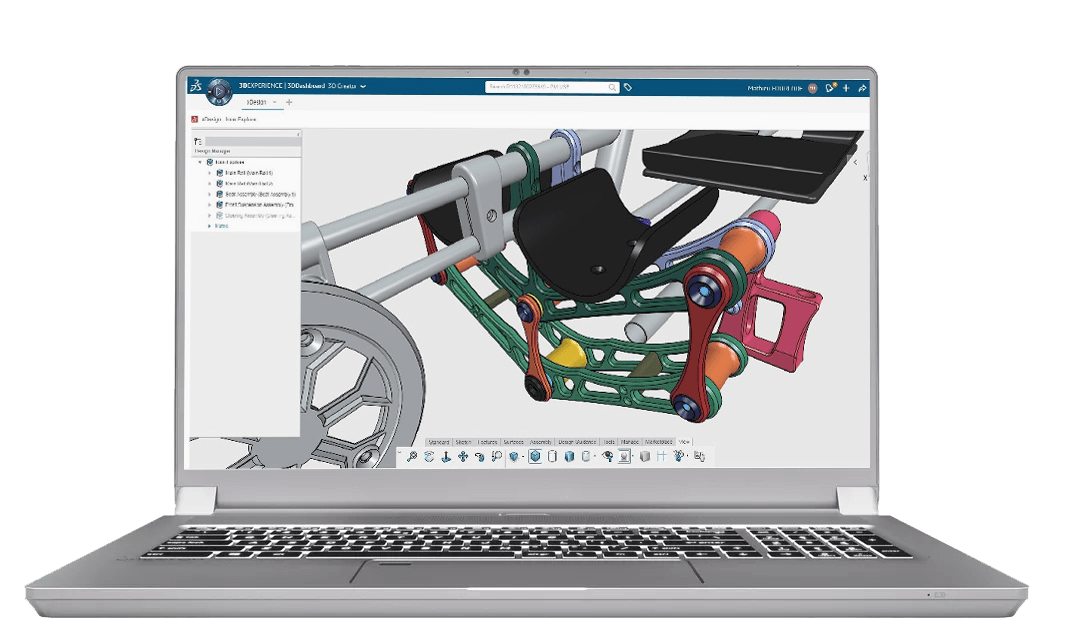
SOLIDWORKS 2024: Top 10 Enhancements
Solutions
Resources & Tutorials
15 January 2024
Ease-of-use has been a cornerstone of the SOLIDWORKS experience from day one. SOLIDWORKS 2024 continues this tradition, incorporating user feedback into enhanced functionalities and time saving features. Applications Engineer, Sam Barlow, picks out ten of the best...